The effect of SENSE Theatre as a therapy on language delays in children with Autism Spectrum Disorder
ABSTRACT
One in 68 children have Autism spectrum disorder, ASD, and many have affected daily lives (19). ASD is a neurodevelopmental disorder that is characterized by restricted behavior, difficulty in social ability, and communication (1). Many of these children also struggle with language ability as some are nonverbal or have limited verbal ability (3). There is no cure, but there are several treatments such as therapies and medication. Most of these, however, have adverse side effects or have little research available on them (7). A possible alternative treatment to medications is a peer-mediated theatre intervention known as SENSE Theatre. The treatment aims to help participants develop social skills, reduce stress, and increase communication ability. The social aspect of the intervention has been evaluated, so the possible changes in language ability are now being studied (8). By using psychological tests that measure basic communication, symptom severity, and verbal bout and linguistic test that measures verbal recall, it was determined that SENSE can be an effective treatment for language delays in children with ASD. Two of the more specific tests (measures of symptom severity and verbal bout) showed a significance while the other less specific tests showed a possible correlation but were not significant.
INTRODUCTION.
Autism spectrum disorder (ASD) is a neurodevelopmental disorder that includes symptoms such as limited social interaction, difficulty in verbal and nonverbal communication, and restricted interests (1). Many children begin to display symptoms as early as twelve to twenty-four months (2). Previous research has shown that children with ASD tend to score lower in language ability such as speech development, semantic understanding, and expressive language, than typically developing (TD) children. This may be why children with ASD struggle with social communication and interaction (3). While there is literature on language ability in children with ASD, few studies focus on the effect therapies have on it (4). Some studies focus on identifying the range of language delay in children with ASD as it can vary from fully functional to non-verbal (3). Others use brain imaging to investigate possible underlying structural components to language delays in children with ASD, such as investigating the correlation between language ability and functional connectivity in the brain (5).
While there are many potential treatments for ASD, there is no cure. One common treatment is the use of drugs such as Risperidone, an antipsychotic, which treats behavioral symptoms such as hypersensitivity and disruptive behaviors (6). While these may lessen a child’s symptoms, many parents worry about the safety and side effects of constant drug use as a form of treatment. Because of this, parents have turned to alternative medicine such as acupuncture, vitamins, and ketogenic diets (7). These can potentially lessen symptoms, but in most cases they are not effective enough nor have they been studied thoroughly enough to be assumed risk free (7). These treatments have been used in combination with therapies such as occupational or speech therapy (8). While these have successes, most children have many types of therapy because most only treat specific symptoms (9)
One possible treatment that aims to combine therapies such as speech and occupational is SENSE, Social Emotional NeuroScience Endocrinology, Theatre. SENSE Theatre is a peer-mediated therapy for children with ASD. It is a theatre intervention focused on increasing social ability and communication in children with ASD through the use of peers. During the 10-session intervention, participants are paired with a TD, trained peer, who teaches appropriate social interaction through modeling and theatre techniques. While the other therapies focus on a single element of treatment, SENSE aims to combine music and theatre to work on communication and social interaction (9). Previous research shows that SENSE can increase memory for faces and other areas of social competence in children with ASD (10). It is still unclear, however, which parts of the treatment are most effective and if SENSE is effective for all children with ASD.
The use of theatre techniques in SENSE has shown to increase reciprocal social communication (2). Social and linguistic ability may increase due to interaction that is encouraged during SENSE. This study aims to measure any changes in language ability following SENSE. It is hypothesized that there are measurable effects on verbal ability and verbal recall. This could help with further testing of language ability in children with ASD as well as to show more research towards SENSE being an effective therapy for children with ASD.
METHODS.
Participants.
Eighty-one children with ASD were randomly assigned to experimental (EXP; N=44) and waitlist control (WLC; N=37) groups across three cohorts, these being the years of 2014, 2015, 2016 where participants were on the waitlist or received treatment. Age ranged from 7-16 (mean age (M) =11.06). Intellectual ability (IQ) was measured using the Wechsler Abbreviated Scale of Intelligence (WASI) (11). Diagnosis was based on DSM-V criteria confirmed by a clinical psychologist and corroborated by the Autism Diagnostic Observation Schedule (ADOS) (12). An Institutional Review Board approved this study. Written informed consent was obtained from the parents and the children provided written and verbal assent.
Procedure.
Both the EXP and WLC groups were given the Adaptive Behavior Assessment Scale (ABAS), Clinical Evaluation of Language Fundamentals (CELF), Social Responsiveness Scale (SRS), and Peer Interaction Paradigm (PIP) before and after the 10-week intervention period. The pre-tests (before the 10 week intervention) were used as the baseline and the post-tests (after the 10 week intervention) were the treatment values. All tests were administered according to standard protocol. Due to the wide range of verbal and skill ability of the children, not all participants took every test as the EXP CELF measure had only 28 participants able to complete it.
Psychological Measures.
The Adaptive Behavior Assessment Scale (ABAS) is a parent report of a child’s behaviors to identify problems relating to social skills, communication, and daily life. The Communication Subscale was used, which measures the child’s skills relating to communication with others. The test asks broad questions to establish the child’s basic ability to communicate such as ‘Does your child ask questions in class?’ (13).
The Social Responsiveness Scale (SRS) is a parent report that measures the severity of ASD symptoms in children. The Social Communication subscale was used, which measures the child’s ability to communicate with others effectively and appropriately. It is a measure specific to children with ASD so it presents the parent with specific questions to identify the depth of the child’s language impairment such as ‘How does your child react to conflict?’ (14).
Language Measures.
The Clinical Evaluation of Language Fundamentals (CELF) is a comprehensive measure of language ability. The Repeating Sentences subscale was used, which measures a child’s verbal recall. The test requires the proctor to state a sentence and then have the child repeat the sentence verbatim as sentences increase in difficulty both in length and complexity (15).
Peer Interaction Paradigm.
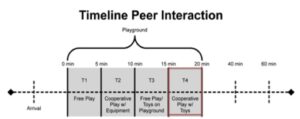
The Peer Interaction Paradigm (PIP) is an ecologically valid play observation. Two novel peers facilitate play with the participant for a total of 20 minutes. Two 5-minute periods consist of free play (T1, T3) and two five-minute periods of cooperative play with the peers (T2, T4) (Figure 1). For this study, the T4 Verbal Bout (duration of reciprocal verbal exchange with a novel peer) was used. The percentage of verbal bout was analyzed (16).
Figure 1. Peer Interaction Paradigm (PIP) Timeline (17).
Statistical Analysis.
T-tests were performed on Age, ADOS score, and IQ before intervention to control for group differences. ANCOVAS were run for the ABAS, CELF, SRS, and PIP. Post, test scores following SENSE or control period, was used as the dependent measure while pre, test scores prior to SENSE or control period, was covariate.
RESULTS.
Demographics.
T-tests were used to determine that there were no significant between-group differences in age or ADOS score; all p-values were >0.05. T-tests revealed a significant between-group difference in which the experimental group values were greater than the waitlist control group values in IQ as measured on the WASI (t(79)=-2.66, p=0.01.
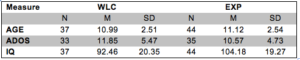
Each participant was randomly assigned to either experimental or waitlist control groups. These participants represent three different cohorts and the demographics for each group are included in Table 1. The table shows that the waitlist control group had 37 participants while the experimental group had 44 participants.
Table 1. Demographics shown include sample size (N), mean (M), and standard deviation (SD).
By comparing the waitlist group to the treatment group on each test, ABAS, CELF, SRS, and PIP, it can be identified which group did better. Ideally, the treatment group will do significantly better on the tests than the waitlist group, which would indicate that the treatment had some positive effect on the participants.
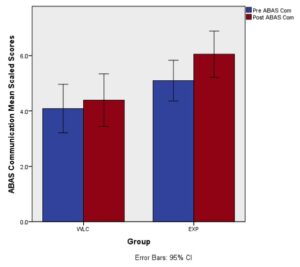
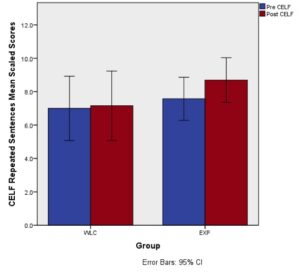
Results of ANCOVAs showed that there were no significant differences between EXP and WLC groups on the ABAS Communication (F(1,76)=3.66, p=0.06), or CELF- Repeating Sentences (F(1,68)=2.95, p=0.09) following treatment while controlling for pre-intervention scores.
Analysis revealed no significant changes in ABAS scores between the experimental and waitlist groups, pre versus post scores. This shows that there was no significant increase in communicative ability following SENSE, however, the p-value is close to being acceptable for significance so with more subjects and future testing, this measure may become significant (F(1,76)=3.66, p=0.06).
Analysis showed no significant increases in verbal recall on the CELF (F(1,68)=2.95, p=0.09). This indicates that verbal recall was not increased following SENSE Theatre.
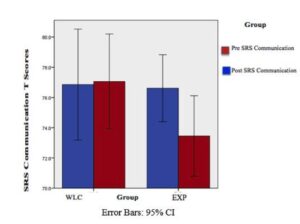
Analysis revealed significant improvement in SRS scores following treatment (F(1, 75)=3.81, p=0.05). This demonstrates that participants in the experimental group, those who received treatment, experienced a decrease in severity of various symptoms following SENSE. The scores for the waitlist control group were relatively the same in pre and post testing as the t score, or standardized combination of each participants’ scores, were close to the same before and after then control period (Figure 2).
Figure 2. Severity of symptoms decrease following treatment, pre-SRS shown in blue, post SRS shown in red p=0.05 (Waitlist: N=34, M=77.06, SD=9.00) (Treatment: N=44, M73.46, SD= 8.98, error bars= 95% confident)
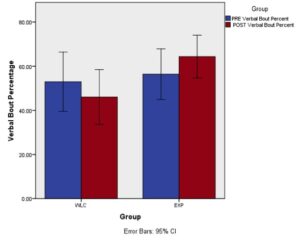
Analysis revealed a significant improvement in amount of verbal bout on the PIP (T4) (F(1, 77)=5.97, p=0.02). This shows that there was an effect of treatment on verbal bout following SENSE Theatre (Figure 3).
Figure 3. Increase in verbal bout during PIP at T4 following treatment, pre-verbal bout shown in blue, post verbal bout shown in red (p=0.02) (Waitlist: N=37, M=46.04, SD=37.23) (Treatment: N=43, M=64.37, SD=31.50, error bars= 95% confident)
DISCUSSION.
The current study found that SENSE Theatre may have a significant effect on language delays in children with ASD. The PIP showed that children were more likely to engage in verbal bout with another child following SENSE. This shows SENSE could have a positive effect on language delays. This is the most direct measure used, as it is an accurate measure of how much the child spoke rather than a general measure of language ability.
The SRS showed that there was a significant decrease in symptom severity such as aggression or social anxiety, in children with ASD following SENSE. As high scores indicate more severe symptoms, the decrease in scores shows an improvement in symptom severity [16]. This shows that the participants could also have a significant increase in language ability as the symptoms that are reported on the SRS include possible language and social deficits. The SRS is a parent measure rather than a direct measure like the PIP, but it is still a highly effective measure.
The ABAS and the CELF were not statistically different between groups, but they were trend line meaning that with future testing these could show an increase in language ability. Currently, however, the overall behavior of the child did not increase after SENSE according to ABAS. The CELF showed that there was no change in scores following SENSE. This could be because the measure only looks at a child’s ability to recall sentences. While SENSE does work on theatre lines, there is not direct practice of repeating sentences.
CONCLUSION.
The main symptoms of children with ASD include difficulty in social functioning, interaction, and communication including language delays. There are many possible treatments to lessen these symptoms, however, there is no cure. Some parents may want an alternative to medications so therapies that can reduce their child’s symptoms are important (7). SENSE could be a possible therapy to replace these medications and therapies.
The current study found that there were significant changes in language ability following SENSE Theatre with the use of direct measure and a symptom severity parent measure. The PIP and the SRS showed significant increases in verbal bout and decreases in symptom severity, respectively. This shows that SENSE could be a therapy for language delays in children with ASD.
The study had limitations. The most significant was sample size. The groups were not equal in size. This could have made the results more varied. There was also a large age range, which could vary the results slightly, but isn’t significant enough to majorly affect the data. Finally, there was a large range of IQs between the groups. As IQ can affect language ability, this could also affect the results. One future direction is to compare the language ability of participants in SENSE to patients who receive speech therapy to see if the language ability is being increased as much as it may be increase due to a therapy focused on language. Traditional therapies help children with ASD to develop skills such as language ability, but also help with coping and developing social skills. In one study, up to seventy percent of parents said that traditional therapy helped their child significantly (18).
The current study aimed to evaluate the effectiveness of a possible therapy on language delays in children with ASD. It was found that SENSE can increase language ability in children with ASD using a direct measure of verbal bout and a parent measure of symptom severity. As ASD continues to become a prevalent disorder, there is a need for therapies that help children increase social ability and communication. If it can be understood what treatments work best for children with ASD, a cure or the cause could possibly be found. SENSE Theatre is a novel therapy that needs more research to determine its effectiveness and why it is effective for each child. This makes research on SENSE important and necessary to help develop the best possible therapy.
ACKNOWLEDGMENTS.
I would like to thank the SSMV staff, especially Dr. Muller for all of his guidance. I would also like to thank Ian Muse for his help and the families and children for their participation in this study.
SUPPORTING INFORMATION.
Supplemental Figure 1 is a graph of the ABAS Communication subscale showing a lack of improvement in scores.
Supplemental Figure 2 is a graph of the CELF Repeating Sentences showing a lack of improvement in verbal recall.
REFERENCES.
- APA. Diagnostic and statistical manual of mental disorders, Fifth Edition (DSM-5). Washington, D.C.: American Psychiatric Association (2013).
- Rogers, S., & DiLalla, D. Age of Symptom Onset in Young Children with Pervasive Developmental Disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 29, 863-872 (1999).
- Lewis, F., Murdoch, B., Woodyatt, G. Linguistic abilities in children with autism spectrum disorder. Research in Autism Spectrum Disorders. 1, 85-100 (2007).
- Kjelgaard, M. M., & Tager-Flusberg, H. An Investigation of Language Impairment in Autism: Implications for Genetic Subgroups. Language and Cognitive Processes. 16, 287–308. (2001).
- Verly, M., Verhoeven, J., et al. Structural and Functional Underconnectivity as a Negative Predictor for Language in Autism. Human Brain Mapping, 35, 3602–3615 (2014).
- Canitano, R., & Scandurra, V. Risperidone in the treatment of behavioral disorders associated with autism in children and adolescents. Neuropsychiatric Disease and Treatment, 4, 723–730 (2008)
- Lofthouse, N., Hendren, R., et al. A Review of Complementary and Alternative Treatments for Autism Spectrum Disorders. Autism Research and Treatment 2012 (2012).
- Corbett, B. A., Qualls, L. R., et al. Peer-Mediated Theatrical Engagement for Improving Reciprocal Social Interaction in Autism Spectrum Disorder. Frontiers in Pediatrics. 2, 110. (2014).
- Levy, S. E., & Hyman, S. L. Complementary and Alternative Medicine Treatments for Children with Autism Spectrum Disorders. Child and Adolescent Psychiatric Clinics of North America. 17. 803–ix. (2008).
- Corbett, B. A., Key, A. P., et al. Improvement in Social Competence Using a Randomized Trial of a Theatre Intervention for Children with Autism Spectrum Disorder. Journal of Autism and Developmental Disorders. 46, 648-672 (2016).
- McCrimmon, A. W., Smith, A. D. Review of the Wechsler Abbreviated Scale of Intelligence, Second Edition (WASI-II). Journal of Psychoeducational Assessment. 31, 337-341 (2012).
- Lord, C., Risi, S., Lambrecht, L. et al. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. J Autism Dev Disorder 30, 205-223 (2000).
- Rust, J. O., Wallace, M. A., Review of Adaptive Behavior Assesment System-Second Edition. Journal of Psychoeducational Assessment,22, 367-373 (2004).
- Constantino, J. N., & Gruber, C. P. Social Responsiveness Scale. Los Angeles: Western Psychological Services. (2005).
- Paslawski, T. The Clinical Evaluation of Language Fundamentals, Fourth Edition (CELF-4). Canadian Journal of School Psychology. 20, 29-134 (2005).
- Corbett, B. A., Swain, D. M., et al. Biobehavioral profiles of arousal and social motivation in autism spectrum disorders. J Child Psychol Psychiatry. 55, 924–934 (2014).
- Corbett, B. A., Muscatello, R. A., & Blain, S. D. Impact of Sensory Sensitivity on Physiological Stress Response and Novel Peer Interaction in Children with and without Autism Spectrum Disorder. Frontiers in Neuroscience. 10, 278. (2016).
- Goin-Kochel, R. P., Mackintosh, V. H., Myers, B. J. Parental reports on the efficacy of treatments and therapies for their children with autism spectrum disorders. Research in Autism Spectrum Disorders. 3, 528-537 (2009).
- CDC estimates 1 in 68 children has been identified with autism spectrum disorder. Center for Disease Control and Prevention. (2014).
Posted by John Lee on Tuesday, December 22, 2020 in May 2018.
Tags: Autism, Language, SENSE Theatre, Therapy