Pregnancy and COVID-19: The impact on prenatal care and maternal outcomes
ABSTRACT
The SARS-CoV-2 (COVID-19) pandemic has strained healthcare systems around the world, impacting maternal characteristics and outcomes, most notably adequacy of prenatal care and modes of delivery. The primary goal of our study is to assess the changes in initiation of prenatal care, adequacy of prenatal care utilization, and cesarean delivery during the COVID-19 pandemic in years 2020-2022 in comparison to prior years (2019). We assessed the changes in five measures of prenatal care and two outcomes related to C-section by computing unadjusted logistic regressions and calculating the marginal effects for each year. Compared to 2019, there was a significant decrease in Adequate Plus Prenatal Care utilization, in Less Adequate Prenatal Care utilization, and Adequate Prenatal Care utilization in all subsequent years. Additionally, there were increases in both C-section and Low Risk C-section procedures in 2020, 2021, and 2022.
INTRODUCTION.
The SARS-CoV-2 (COVID-19) pandemic has strained healthcare systems around the world and placed stressors on pregnant persons. There were 3,613,647 births in the United States (U.S.) in 2020 [1]. Recent data states that pregnant or recently pregnant persons are more likely to become seriously ill from COVID-19 [2]. A global scoping review including 95 articles published from January 1st, 2020 to September 11th, 2020, regarding maternal and perinatal health, reported decreased numbers of prenatal care visits, strained health infrastructure, severely higher percentages of maternal mental health issues such as clinical anxiety and depression, policies surrounding pregnancy implemented without adequate evidence, and increased incidence of domestic violence [3].
Pregnant persons with COVID-19 are more likely to experience complications in pregnancy, as they have a higher chance of delivering a preterm or stillborn infant [4]. Increased C-section rates have been found to be connected to pregnant persons with COVID-19 [5]. Procedures were implemented to prevent transmission from pregnant persons with COVID-19 [3]. Data sent to the CDC as a part of COVID-19 surveillance efforts show that from January 22nd to June 7th, out of the 91,412 women aged 15-44 with laboratory-confirmed SARS-CoV-2 infections and the 8,207 among those who were pregnant, 31.5% of pregnant persons were hospitalized while 5.8% of non-pregnant women were hospitalized [4].
Pregnant persons with COVID-19 also had higher ICU admission rates and required mechanical ventilation more often than non-pregnant women [4]. Despite hospitalizations being more prevalent among pregnant persons, mortality rates among pregnant persons and non-pregnant women were the same at 0.2% [4].
Literature since the start of the pandemic has started to explore the differences in maternal and infant care delivery and outcomes. Studies outside of the U.S. found similar maternal characteristics and small changes in pregnancy outcomes from between designated pre-pandemic periods and pandemic periods. A study conducted in the United Kingdom assessing 948,020 births found that maternal characteristics (i.e. age, gravidity or pregnancy history, comorbidities or having two or more medical conditions, and COVID-19 status of the person delivering at time of birth) did not statistically change from March 23rd, 2019 to February 22nd, 2021 [6].
The United Kingdom study [6] found marginally lower percentages of preterm birth from 6.1% in March 23rd 2019 to February 22nd, 2020, and 6.0% in March 23rd, 2020 to February 22nd, 2021. Also, small for gestational age (SGA) births increased from 5.8% in March 23rd, 2019 to February 22nd, 2020 to 5.6% in March 23rd, 2020 to February 22nd, 2021 over the period of one year [6]. Slightly higher percentages of obstetric intervention were discovered (i.e., measures taken to deliver the infant including induction, epidural use, episiotomy, instrumental delivery, and cesarean delivery) [6, 7]. A study conducted in Iran that included 2,503 pregnant persons, 51.4% who were admitted to the hospital before the COVID-19 lockdown and 48.6% who were admitted during the COVID-19 lockdown, showed a decrease in preterm birth and low birthweight with higher rates of ICU admission and consistent stillbirth levels from February 2019 to April 19th, 2020 [8].
Inside of the U.S., changes were found in certain pregnancy outcomes while no changes were found in others. A national study of 1,277,713 deliveries from 2019-2020 revealed that rates of ICU admission and preterm birth decreased while all other outcomes measured remained the same [9]. In another national study evaluating adverse pregnancy outcomes of 324,998 births from January 1st, 2019 to December 31st, 2020, there were significantly higher rates of gestational diabetes, gestational hypertension, poor fetal growth, and preeclampsia in the pandemic period (January 2020-January 2021) compared with the pre pandemic period (January 2019-January 2020) [10].
The primary goal of our study is to assess the changes in initiation of prenatal care, adequacy of prenatal care utilization, and cesarean delivery during the COVID-19 pandemic in years 2020-2022 in comparison to prior years (2019). We hope to find trends in the occurrences of these factors over time, to analyze how these trends relate to one another, as well as to determine the root cause of these patterns. It is important to ask these questions because they serve as markers for pregnancy outcomes and complications such as maternal mortality and morbidity. In this study, we are asking one fundamental question: Did the COVID-19 pandemic have an adverse effect on prenatal care quality and C-section rates in the U.S.?
MATERIALS AND METHODS.
Data: In this retrospective study, we assessed publicly available, nationwide pregnancy data from the Centers for Disease Control and Prevention (CDC) and the National Center for Health Statistics, National Vital Statistics System on Natality. Our primary dataset included selected medical and health characteristics of births, by month of birth in the United States from January of 2019 through March of 2022. The data includes provisional estimates for 2021 (99.96% of births) and 2022 (99.53% of births). The maternal characteristics assessed were: prenatal care beginning in the first trimester, late or no prenatal care, adequacy of prenatal care utilization (adequate, adequate plus, and less than adequate), total cesarean delivery, and low-risk cesarean delivery.
Variables: Late or no prenatal care is defined by prenatal care that began in the third trimester and no prenatal care. Adequacy of prenatal care utilization is based on the Adequacy of Prenatal Care Utilization Index. Adequate plus prenatal care is prenatal care beginning by the fourth month of pregnancy and including 110% or more of the recommended number of visits. Adequate prenatal care is defined as prenatal care beginning by the fourth month of pregnancy and including at least 80%-109% of the recommended number of visits. Less than adequate prenatal care is defined as prenatal care beginning after the fourth month of pregnancy or including less than 50% of the recommended number of visits.
Analysis: We assessed the changes in maternal characteristics and outcomes by computing unadjusted logistic regressions for each and calculating the marginal effects (ME) (percentage point difference in probability from the baseline) across each year of the study (i.e., 2019-2022). Statistical analysis was conducted using Stata version 17.0. Marginal effects are expressed as percentages and comparison of outcomes was performed using Fisher’s Exact test (p<0.05).
RESULTS.
All results are summarized in Table 1.
| Table 1. Probability of Maternal Outcomes During COVID-19 Pandemic Periods (2020, 2021, 2022) Relative to Pre-Pandemic Period (2019) | |||||
| Condition/Measure | Period | Percent Change From 2019 | 95% CI – Upper | 95% CI – Lower | Corresponding Figures |
| Prenatal Care – 1st Trimester | 2020 | 0.12% | -0.48814 | 0.72147 | Figure S4 |
| 2021 | 0.76% | 0.15353 | 1.36314 | ||
| 2022 | -0.61% | -1.56461 | 0.34794 | ||
| No/Late Prenatal Care | 2020 | -0.18% | -0.37996 | 0.01329 | Figure S3 |
| 2021 | -0.10% | -0.29663 | 0.09663 | ||
| 2022 | 0.23% | -0.07756 | 0.54423 | ||
| Adequate Plus Prenatal Care | 2020 | -3.13% | -4.15571 | -2.09429 | Figure 1 |
| 2021 | -2.23% | -3.26404 | -1.20263 | ||
| 2022 | -3.06% | -4.68802 | -1.42864 | ||
| Adequate Prenatal Care | 2020 | 1.13% | 0.65987 | 1.6068 | Figure S2 |
| 2021 | 1.09% | 0.6182 | 1.56513 | ||
| 2022 | 0.92% | 0.16805 | 1.66528 | ||
| Less Adequate Prenatal Care | 2020 | 1.98% | 1.18537 | 2.7813 | Figure S1 |
| 2021 | 1.14% | 0.3437 | 1.93963 | ||
| 2022 | 2.14% | 0.87997 | 3.40336 | ||
| C-Section | 2020 | 0.13% | -0.10226 | 0.35226 | Figure S5 |
| 2021 | 0.43% | 0.19774 | 0.65226 | ||
| 2022 | 0.47% | 0.10734 | 0.826 | ||
| Low-Risk C-Section | 2020 | 0.28% | 0.08758 | 0.47908 | Figure 2 |
| 2021 | 0.71% | 0.51258 | 0.90408 | ||
| 2022 | 0.67% | 0.35716 | 0.97618 | ||
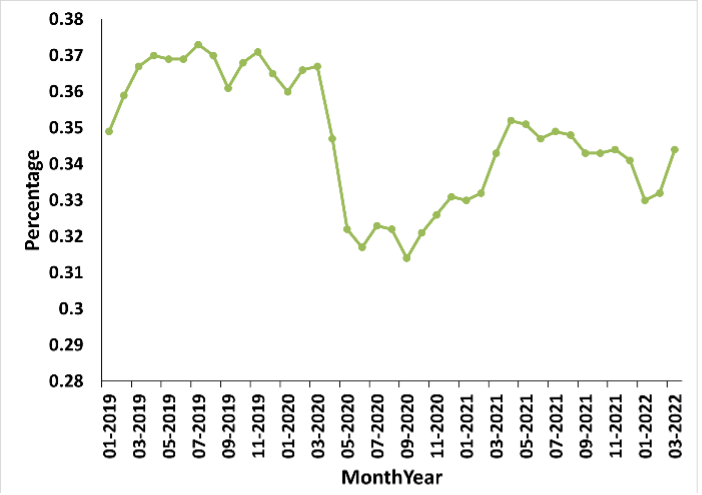
Adequate Plus Prenatal Care utilization in the United States decreased during the pandemic periods (2020, 2021, and 2022) compared to the pre-pandemic period (2019), with -3.13% difference 2020, a -2.23% difference in 2021, and a -3.06% difference 2022 (Figure 1).
Figure 1. Trends over time in adequate plus prenatal care utilization show a decrease in the probability of receiving this level of care in all pandemic periods when compared to 2019.
A significant increase in Less Than Adequate Prenatal Care utilization was found between COVID-19 pandemic periods and the pre-pandemic period (Fig. S1). The increase in probability for this category was 1.98% in 2020, 1.14% in 2021, and 2.14% in 2022. There were also significant increases found in percentages of Adequate Prenatal Care utilization (Fig. S2) with a 1.13% difference in 2020, a 1.09% difference in 2021, and a 0.92% difference in 2022.
Small differences were found in percentages of No/Late Prenatal Care utilization between pandemic and pre-pandemic periods (Fig. S3). In 2020 there was a -0.18% difference, in 2021 there was a -0.10% difference, and in 2022 there was a 0.23% difference.
Percentages of Prenatal Care – 1st Trimester utilization fluctuated during pandemic periods compared to the pre-pandemic period (Fig. S4). For 2020 there was a 0.12% change, for 2021 there was a 0.76% change, and for 2022 there was a -0.61% change.
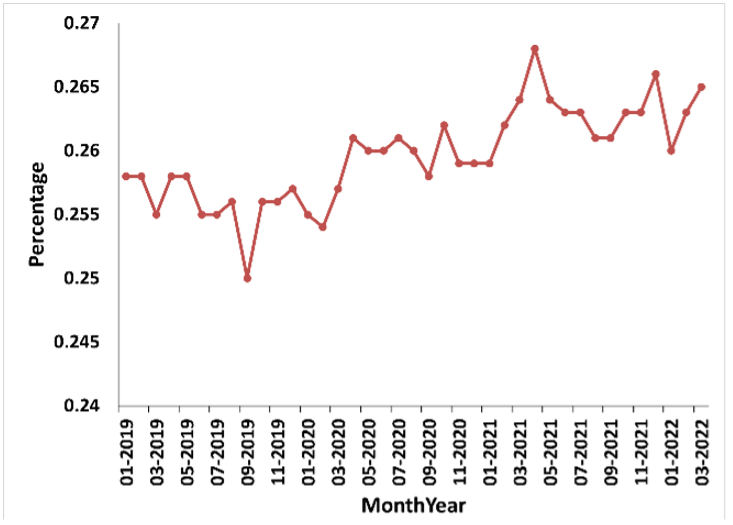
The frequency of C-Section procedures in the U.S. increased, especially in the last two pandemic periods (2021 and 2022) compared to the pre-pandemic period (Fig. S5). There was a difference of 0.13% found in 2020, a 0.43% difference found in 2021, and a 0.47% difference found in 2022. Similar to overall C-Section procedure percentages, Low Risk C-Section percentages increased throughout the pandemic period, especially in the years 2021 and 2022. For 2020 a change of 0.28% was found, for 2021 a 0.71% change was found, and for 2022 a 0.67% change was found (Figure 2).
Figure 2. Trends over time in low-risk cesarean delivery present an increase in the probability of this maternal outcome in all pandemic periods compared to the year of 2019.
DISCUSSION.
There were three significant findings from our body of work: (1) When compared to the pre-pandemic period of 2019, there was a significant decrease in Adequate Plus Prenatal Care utilization in 2020, 2021, and 2022, (2) Increases in Less Adequate Prenatal Care utilization and Adequate Prenatal Care utilization were found between the pre-pandemic period of 2019 and the pandemic periods of 2020, 2021, and 2022, and (3) Compared to the pre-pandemic period of 2019, there were increases in both C-section and Low Risk C-section procedures in 2020, 2021, and 2022.
Our findings show that the COVID-19 pandemic negatively impacted the quality of overall prenatal care utilization in the U.S. There was a significant decrease in Adequate Plus Prenatal Care utilization between the COVID-19 pandemic periods (2020, 2021, and 2022) in relation to the pre-pandemic period (2019) which caused significant increases in percentages of both Less Adequate Prenatal Care utilization and Adequate Prenatal Care utilization. This reflects the findings of Kotlar et al., who found decreases in the overall global number of prenatal care visits due to the pandemic [3]. Small changes were found in No/Late Prenatal Care utilization and there were fluctuations in Prenatal Care – 1st Trimester utilization from pandemic periods compared to the pre-pandemic period. Both percentages of C-Section and Low Risk C-Section increased in pandemic periods compared to the pre-pandemic period, especially in the years of 2021 and 2022.
This aligns with the findings of Gurol-Urganci et al. who found small increases in elective and emergency C-section rates from 2019 to 2021 [6]. C-section procedures lead to longer hospital stays and recovery times and bring the risks of a major surgery, including severe bleeding, scarring, infection, reaction to anesthesia and a longer duration of pain. Percentages of maternal morbidity and mortality of C-section procedures are higher due to blood clots, infections, and reactions of anesthesia than that of vaginal birth [11]. C-sections bring in more money to hospitals and can be scheduled in advance at times that are convenient for both the patient and the healthcare workers. This can be used in times of COVID-19 when healthcare infrastructure is stressed to make the job easier for OB-GYNs as well as to make more money, however it also puts the well-being of the patient at risk.
The major limitation of our research is that it is an unadjusted analysis which does not account for other factors that may have impacted maternal characteristics from 2019-2022, which introduces bias as to what factors played the most impactful role on maternal characteristics–in this case, the COVID-19 pandemic. The dataset used in this paper presents percentages and not rates, which only accounts for the amount of patients with the measured maternal characteristics or outcomes and not the frequency in occurrence of the specific characteristic or outcome. This research only represents the U.S. and cannot represent anywhere past U.S. borders. There is also no comparison between the U.S. as a whole versus the average state in the U.S.
Strengths of this paper include the importance of analyzing maternal characteristics and outcomes, especially in a time period as unique as a pandemic. Looking at trends in maternal care and their outcomes allows for the prediction of maternal health in future periods of stress in healthcare infrastructure to better address the needs of pregnant persons, which can decrease rates of mortality and morbidity.
CONCLUSION.
To conclude, the overall quality of prenatal care in the U.S. decreased and both C-section and low risk C-section procedures increased during pandemic periods (2020, 2021, 2022) relative to the reference year (2019) due to the COVID-19 pandemic. Our research can be used by pregnant persons, policy-makers, and key stakeholders in the United States and beyond to make more informed decisions regarding maternal health. Resources should be available to maintain the quality of prenatal care during times of emergency, and low risk C-section procedures should not happen solely for the convenience of healthcare workers even under times of pressure, as it puts the wellbeing of the patient at greater risk.
ACKNOWLEDGMENTS.
I would like to thank my mentor Kathryn Thompson of Brown University for her guidance and support throughout this project as well as for teaching me how to find the story behind the numbers. I would also like to thank the Lumiere Program for their work in fostering student research.
SUPPORTING INFORMATION.
Supporting information includes additional figures illustrating trends of primary outcomes over time (Figures S1-S5, Table S1).
REFERENCES
- Osterman MJK, Hamilton BE, Martin JA, Driscoll AK, Valenzuela CP. Births: Final data for 2020. National Vital Statistics Reports. 70(17), 1–2 (2022).
- Pregnant and Recently Pregnant People. 2022. Centers for Disease Control and Prevention: Centers for Disease Control and Prevention; [March 3rd, 2022; July 21st, 2022].
- Kotlar B, Gerson E, Petrillo S, Langer A, Tiemeier H. The impact of the COVID-19 pandemic on maternal and perinatal health: a scoping review. Reprod Health. 18(10), 1–34 (2021).
- Ellington S, Strid P, Tong VT, Woodworth K, Galang RR, Zambrano LD, Nahabedian J, Anderson K, Gilboa SM. Characteristics of Women of Reproductive Age with Laboratory-Confirmed SARS-CoV-2 Infection by Pregnancy Status — United States, January 22–June 7, 2020. MMWR. 69(25), 769–775 (2020).
- Badran EF, Darwish RM, Khader Y, AlMasri R, Jaberi MA, AlMasri M, AlSa’di F, Yosef LA, al-Badaineh N. Adverse pregnancy outcomes during the COVID-19 lockdown. A descriptive study. BMC Pregnancy Childbirth. 21(761), 2–4 (2021).
- Gurol-Urganci I, Waite L, Webster K, Jardine J, Carroll F, Dunn G, Frémeaux A, Harris T, Hawdon J, Muller P, et al. Obstetric interventions and pregnancy outcomes during the COVID-19 pandemic in England: A nationwide cohort study. PLoSMed. 19(1), 6–8 (2022).
- Dahlen HG, Tracy S, Tracy M, Bisits A, Brown C, Thornton C. Rates of obstetric intervention and associated perinatal mortality and morbidity among low-risk women giving birth in private and public hospitals in NSW (2000–2008): a linked data population-based cohort study. BMJ Open. 4(4), 1–3 (2014).
- Ranjbar F, Allahqoli L, Ahmadi S, Mousavi R, Gharacheh M, Eshragi N, Alkatout I. Changes in pregnancy outcomes during the COVID-19 lockdown in Iran. BMC Pregnancy Childbirth. 21(577), 1–5 (2021).
- Simeone RM, Downing KF, Wallace B, Galang RR, DeSisto CL, Tong VT, Zapata LB, Ko JY, Ellington SR. Changes in rates of adverse pregnancy outcomes during the COVID-19 pandemic: a cross-sectional study in the United States, 2019–2020. J Perinatol. 42(1), 617–623 (2022).
- Sun S, Savitz DA, Wellenius GA. Changes in Adverse Pregnancy Outcomes Associated With the COVID-19 Pandemic in the United States. JAMA Network Open. 4(10), 1–3 (2021).
- Zandvakili F, Rezaie M, Shahoei R, Roshani D. Maternal Outcomes Associated with Caesarean versus Vaginal Delivery. Journal of clinical and diagnostic research. 11(7), 1–3 (2017).
Posted by John Lee on Tuesday, May 30, 2023 in May 2023.
Tags: COVID-19, Maternal Outcomes, Pregnancy, Prenatal Care