Investigating Rising Caesarean Sections in the National Health Service in England
ABSTRACT
A caesarean section (c-section) is an elective or emergency procedure that can occur in place of vaginal birth. C-section rates in the National Health Service (NHS) in England have risen beyond the recommended rate of 10% set by the World Health Organization. Reducing c-section rates is desirable for both maternal and fetal health outcomes, in addition to being a financially beneficial decision for the NHS. This study used the Maternity Monthly Statistics published by the NHS to determine if this data set displayed correlations between named variables and c-section rates. A significant net increase in both elective and emergency c-section rates was found, and mostly significant correlations were found when considering the percentage prevalence of a certain ethnic group or deprivation. These results suggest that the Maternity Monthly Statistics data set shows most of the expected trends, but data privacy restrictions mean that correlations between rates and ethnicity or deprivation might be harder to identify.
INTRODUCTION.
A caesarean section (c-section) is an elective (planned) or emergency procedure that can occur in place of vaginal birth. C-sections can occur for several reasons, such as the baby being in a breech position, pre-eclampsia or in instances of multiple pregnancy. Elective c-sections may occur for clinical reasons; however, they can also be arranged following maternal request. The National Institute for Health and Care Excellence (NICE) states that ‘if, after an informed discussion about the options for birth…the…pregnant person requests a caesarean birth, support their choice’. [1]
The National Health Service (NHS) is a government-funded healthcare system in the United Kingdom, which is free to UK residents at the point of access. The NHS carries out elective c-sections in addition to emergency c-sections.
There are risks associated with c-sections that can be avoided through vaginal birth. The former involves major abdominal surgery (along with its possible complications) and a longer recovery time, in addition to higher associated maternal mortality and increased risk of major bleeding in subsequent pregnancy. [2]
In a statement on c-section rates, the World Health Organization reported that medically justified c-sections can reduce maternal morbidity, but there is no benefit if c-sections occur when the procedure is not medically necessary. Furthermore, no reduction in maternal or newborn mortality rates was found when c-section rates exceed 10% in a population [3] and in England, c-section rates have been rising from about 23% in 2004/5, [4] to 31% in 2019/20. [5] It is therefore beneficial for the NHS to reduce the number of c-sections performed, to improve maternal and newborn health outcomes. As the NHS is a government-funded organization, it is in its interest to reduce costs where possible. One study estimated £9.8 million worth of ‘savings associated with a five-percentage-point change in nulliparous [c-section] rates’. [6]
This paper aims to explore the trends in c-sections rates in the NHS in England, and to establish if a correlation can be found with rising c-section rates and trends in maternal age, ethnicity, and deprivation within the Maternity Monthly Statistics data set.
MATERIALS AND METHODS.
Sample.
This study used data from the NHS Maternity Services Monthly Statistics from September 2017 to December 2022, which is publicly available on their website. 143 NHS trusts (organisational units within the NHS that groups hospitals by region) in England were selected on the basis that they contained the information: number of elective c-sections, number of emergency c-sections, mean maternal age, records of ethnicity and records of deprivation decile of mothers.
Data Processing.
Excel was used to filter suitable trusts. The Maternity Monthly Statistics Excel files for the above range were collated into one table. Additional variables recorded by each trust were filtered out and trusts not containing the named variables were filtered out. VLOOKUP and pivot tables were used to change the formatting of the final table so it could be imported into SPSS. Statistical analysis was done with SPSS ver. 28. Mean percentage of c-sections was calculated from all c-section percentages present for a certain variable (e.g. a mean maternal age of 26.0). Many of the variables were not normally distributed and so Spearman’s rank correlations were used to determine the r values when comparing c-section percentages against percentage ethnicity/deprivation decile.
Resolution of Data.
Due to patient privacy restrictions, the resolution of publicly available NHS data is limited. In the case of the Maternity Monthly Statistics, data was recorded at trust level, rather than individual hospitals. The total number of elective and emergency c-sections per trust was recorded monthly but the other data (maternal age, ethnicity, and deprivation) linked to each of these mothers was pooled with all other women who delivered babies at each trust each month, regardless of method of delivery. However, the named variables above are well documented factors that influence c-section rates both in England and other countries, so this study was carried out to determine if these trends could be seen in this dataset.
RESULTS.
The critical value (where n=6500) when p=0.05 is 0.024.
Figure 1 shows the relationship between mean percentage elective and emergency c-sections and time was mostly positive, with a significant increase in the percentage of both elective and emergency c-sections from September 2017 to September 2022. The mean percentage of emergency c-sections was always greater than that of elective c-sections.
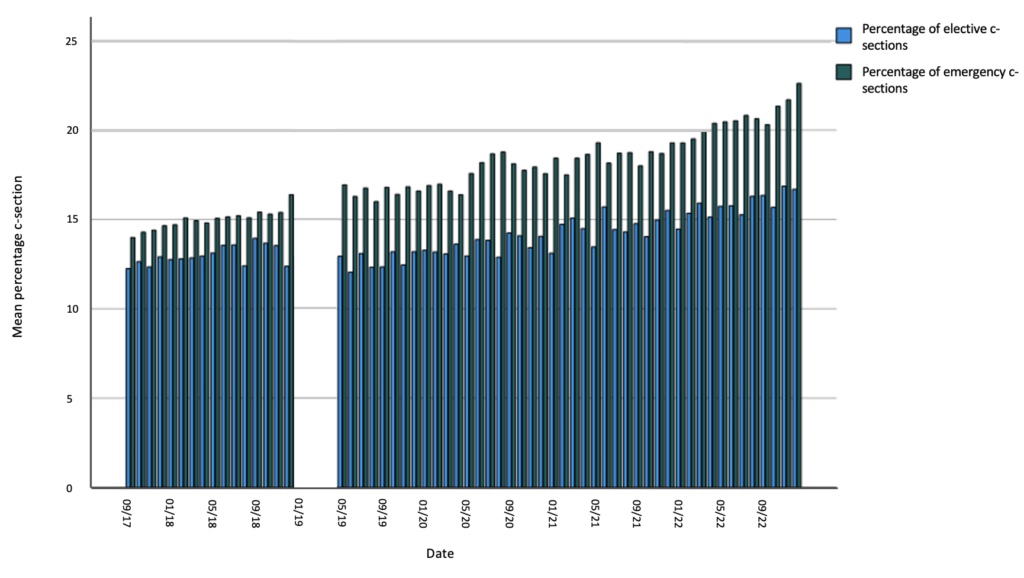
Figure 2 shows a significant increase between increasing maternal age and the mean percentage of elective and emergency c-sections.
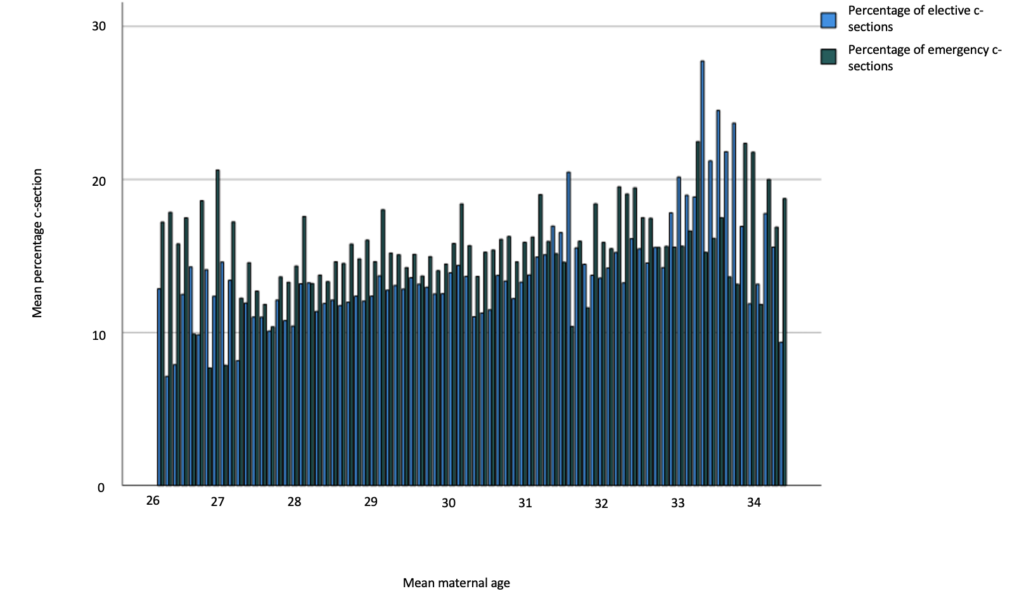
Table 1 shows that for percentage prevalence of an ethnicity or deprivation decile at a trust, the correlation with mean percentage elective and emergency c-section was significant, except in the case of: mean percentage elective c-section against percentage white, deprivation decile 4 and 6; mean percentage emergency c-section against mixed, deprivation decile 1 and 5.
| Table 1. r values determined from Spearman’s rank correlations of percentage prevalence of ethnicity or deprivation in a trust against mean percentage elective or emergency c-section. | ||
| Mean percentage of elective c-section | Mean percentage of emergency c-section | |
| Ethnicity (%) | n = 6782 | n = 6416 |
| Asian/Asian British | 0.080 | 0.329 |
| Other | 0.071 | 0.283 |
| Black/Black British | 0.072 | 0.385 |
| Mixed | -0.091 | -0.058 |
| White | -0.015 | -0.264 |
| Deprivation Decile (%) | n = 6784 | n = 6412 |
| 1- Most Deprived | -0.125 | 0.004 |
| 2 | -0.103 | 0.122 |
| 3 | -0.093 | 0.086 |
| 4 | -0.019 | 0.062 |
| 5 | 0.043 | -0.006 |
| 6 | 0.009 | -0.074 |
| 7 | 0.068 | -0.036 |
| 8 | 0.091 | -0.111 |
| 9 | 0.132 | -0.114 |
| 10- Least Deprived | 0.159 | -0.032 |
DISCUSSION.
Limitations of Dataset.
The main limitation of the Maternity Monthly Statistics data set is the lack of patient level data. While accurate figures for c-section percentages per hospital trust can be obtained, other variables, such as mean maternal age or percentage ethnicity are for the specific trust’s maternity statistics as a whole (i.e. mean maternal age for all births in that trust). Therefore, for maternal age, deprivation and ethnicity, the results must be extrapolated to just births delivered by c-section.
Increase over Time.
Figure 1 shows the expected increase in c-section rates over time, which has been reflected in rates globally [7]. When considering c-sections that aren’t medically necessary, typically those that have occurred due to maternal request, some of the reasons given for this increased rate are: “presumed anxiety or fear of pain from [vaginal delivery] or desire to have a specific day” for birth, as well as “social-cultural and religious regions” which can influence maternally requested c-sections. [7]
Maternal Age.
There are specific risks associated with advanced maternal age (35 years and over) during pregnancy- increased risk of complications like placenta praevia and having stillborn babies. [8] It is expected to see an increase in c-sections, both elective and emergency, as maternal age increases. [9] [10] This increase can be seen in the data set that was selected.
Deprivation Decile.
Deprivation deciles measure the relative areas of deprivation in England, and they consider: income, employment, health deprivation and disability, education, crime, barriers to housing and services, and living environment. ‘Shrinkage estimation is used to improve [the] reliability of the small area data’ to ensure that deprivation deciles are representative of the areas when they contain a small population. The factors considered above are grouped into 5 domains and their scoring is standardised so they ‘are measured from the same metric’. These domains are weighted to indicate their importance (the current weighting has remained constant since 2004) are used to ‘produce an overall relative measure of deprivation’ with decile 1 being the 10% most deprived in England, and decile 10 being the 10% least deprived in England. As the decile is originally based on small geographic areas, scores can be combined to represent a larger geographic area. [11] The r-values calculated from this data set do not show significant correlations between the percentage of mothers from a certain deprivation decile and the percentage of c-sections. However, studies have found that those living in the lowest deprivation deciles have the lowest “odds of having an elective caesarean…but otherwise there is no tendency towards having an elective caesarean section with increasing affluence”. [12] The r-values for deprivation decile 1 and 2 show a stronger correlation between mean percentage of elective c-section than many other deciles, which indicates the opposite of this conclusion. This could be due to the limitations of the data set discussed above.
Ethnicity.
In the Maternity Monthly Statistics, ethnicity was recorded as Asian/Asian British, Black/Black British, White, Mixed and Other. In a study analysing the accuracy of ethnicity records in hospital records versus self-declared records, agreement between hospital and self-declared data sets differed across ethnic groups. “91.3% of women had complete information regarding ethnicity” in hospital statistics but with the “most disagreement…in women coded as mixed in either data set”, so “findings for mixed and other groups…should be treated with caution”. [13] Ethnicity recorded was for all deliveries in the trust, however it will be broadly representative for the population cared for by the trust. In the Maternity Monthly Statistics, ethnicity was a value described by the mother according to a list of options. One study found that “emergency caesarean birth rates were highest in…the black ethnicity groups…and in the [Asian or Asian British] groups (23% and 24% respectively) while elective caesarean birth rates were lowest in the [Black or Black British]…groups”. [14] The correlation between mean percentage of emergency c-sections was strongest in Asian/Asian British and Black/Black British, which is in line with the above conclusion, however the r-values for elective c-sections do not. This could be due to the limitations of the data set discussed above.
CONCLUSION.
In conclusion, many of the expected trends between named variables and c-sections are seen in the Maternity Monthly Statistics data set. The increase in c-sections over time is reflected, and some correlations between ethnicity and deprivation are significant in this data set. It is worth noting the relationship between ethnicity and deprivation decile- some ethnic groups are more likely to fall into certain deprivation deciles, and further research could be done investigating this relationship and c-section rates. Furthermore, because the data relating to maternal age, ethnicity and deprivation does not relate only to c-sections, but all mothers at each trust, these trends could be present in England, but not visible in this data set. The increase in c-sections could therefore be due to the named factors above, or policy changes within the NHS – for example the decision to stop using ‘total caesarean section percentages as a metric’ as ‘maternity units appear to have been penalised for having high caesarean rates’. [15] This investigation supports the importance of data sets with greater resolution, such as the ones mentioned in the Goldacre Review, being available to researchers studying trends in maternal care.
ACKNOWLEDGMENTS.
The author would like to thank Dr Clare Roper for her support and guidance throughout this project.
REFERENCES.
- NICE, “Caesarean birth NICE guideline” (NICE, 2021); https://www. nice.org.uk/guidance/ng192
- M. E. Hannah, Planned elective cesarean section: A reasonable choice for some women? Canadian Medical Association Journal 170, 813-814 (2004).
- WHO, “WHO statement of caesarean section rates” (World Health Organization, 2015); https://www.who.int/publications/i/item/WHO-RHR-15.02
- NHS, “NHS Maternity Statistics- England, 2004-2005” (NHS Digital 2006); https://digital.nhs.uk/data-and-information/publications/statistical/nhs-maternity-statistics/2004-05
- NHS, “NHS Maternity Statistics, England, 2019-20” (NHS Digital 2020); https://digital.nhs.uk/data-and-information/publications/statistical/nhs-maternity-statistics/2019-20
- P. S. Moran et al., Economic implications of reducing caesarean section rates- Analysis of two health systems. PLoS 15, e0228309 (2020).
- C. M. Angolile et al., Global increased caesarean section rates and public health implications: A call to action. Health Science Reports 6, e1274 (2023).
- A. O’Connor, F. Doris, H. Skirton, Midwifery care in the UK for older mothers. British Journal of Midwifery 22, 568-77 (2014).
- L. Herstad et al., Maternal age and elective cesarean section in a low-risk population. Acta Obstetrica et Gynecologica Scandinavica 91, 816-823 (2012).
- S. Y. Kim et al., Effect of maternal age on emergency cesarean section. The Journal of Maternal-Fetal and Neonatal Medicine 33, 3969-3976 (2020).
- Ministry of Housing, “English indices of deprivation 2019: technical report” (Ministry of Housing, Communities and Local Government, 2019); https://www.gov.uk/government/publications/english-indices-of-deprivation-2019-technical-report
- K. Barley, B. Jarman, P. Aylin, A. Bottle, Social class and elective caesareans in the English NHS. The British Medical Journal 328, 1399 (2004).
- J. E. Jardine et al., Validation of ethnicity in administrative hospital data in women giving birth in England: cohort study. British Medical Journal Open 11, e051977 (2021).
- J. H. Bamber et al., A national cohort study to investigate the association between ethnicity and the provision of care in obstetric anaesthesia in England between 2011 and 2021. Anaesthesia 78, 820-829 (2023).
- E. Wilkinson, Hospitals in England are told to stop using caesarean rates to assess performance (BMJ, 2022); https://www.bmj.com/content/376/bmj.o446
Posted by buchanle on Tuesday, April 30, 2024 in May 2024.
Tags: C-sections, NHS, Pregnancy

