Impact of Covid-19 on the Mental Health of Senior Citizens
ABSTRACT
This research paper investigates the impact of the Covid-19 pandemic on the mental health and access to mental health services among senior citizens (aged 50 and older) in St. Mary’s County, Maryland. This study highlights how the pandemic exacerbated existing mental health challenges for older adults who live in a community with limited healthcare resources and a low physician-to-citizen ratio. This is a demographic often overlooked in healthcare discussions. Through surveys conducted at three senior centers, investigators captured the sentiments of senior citizens regarding mental health services before and during the pandemic. Key areas of focus included perceptions of mental health, barriers to accessing mental health treatment, and desired community health resources. Findings indicate a significant deterioration in mental health among seniors during the pandemic, revealing critical gaps in service delivery. This research emphasizes the need for tailored interventions to address the unique characteristics of mental health of seniors in rural areas. In this paper, the researcher proposes strategies to enhance access to mental health care. By identifying location-specific issues, the study aims to contribute to a more comprehensive understanding of senior mental health in the context of Covid-19, facilitating the development of viable solutions for this vulnerable population in St. Mary’s County.
INTRODUCTION.
The 2020s have been defined by the unfolding of a global pandemic, resulting in unparalleled consequences. Not only has Coronavirus (Covid-19) led to the deaths of millions, but various political responses have exacerbated the virus’ destructive effects on countries’ economies and concurrent sociopolitical affairs (1). Pandemics have long-lasting implications on a person’s physical and mental health and tend to affect all demographics differently (2). Covid-19 increased health problems among a particular demographic in St. Mary’s County (3).
St. Mary’s County is located in a rural part of Southern Maryland, with a population of less than 150,000, and an economy that is primarily supported by connections to the Patuxent Naval Base. According to the County Health Ranking Report, “St. Mary’s County is a medically underserved population,” it “has 2,350 citizens per physician, which is less than half the state and national ratios” (4). Consequently, certain groups faced considerable neglect during the pandemic. One such group was the elderly who are often overlooked and unable to get proper access to healthcare, especially mental health treatment. As stated by the World Health Organization (WHO), “due to population aging, the number of senior citizens with mental disorders is expected to double by 2030” (5). As the elderly population continues to grow, it’s crucial that they receive more assistance and attention (6). Though there have been global attempts to address how the pandemic has affected the mental health and treatment of senior citizens, there continues to be a lack of research surrounding the negative impact of Covid-19 had on senior citizens’ mental health in St. Mary’s County (7).
The research conducted in this study analyzed how Covid-19 exacerbated mental health issues and access to mental health treatment for senior citizens (aged 50 and older) living in independent housing facilities within St. Mary’s County. This study will examine how there has been a change in senior citizens’ mental health and access to mental health treatment due to the pandemic. This survey was conducted in 3 senior centers in St. Mary’s County (Northern Senior Center, Loffler Senior Center, and Garvey Senior Center). The goal of the survey was to directly assess independent senior citizens’ opinions regarding this change over time. This survey inquired about senior citizens’ thoughts when they hear the term “mental health”, how they feel about mental health services geared towards senior citizens before and during Covid-19, how they access mental health services, what prevents senior citizens from getting mental health services, and what kind of community health services would be helpful for senior citizens and their mental well-being. The goal of this research is to provide deeper insight into mental health problems present in senior citizens and to find a location-specific solution.
MATERIALS AND METHODS.
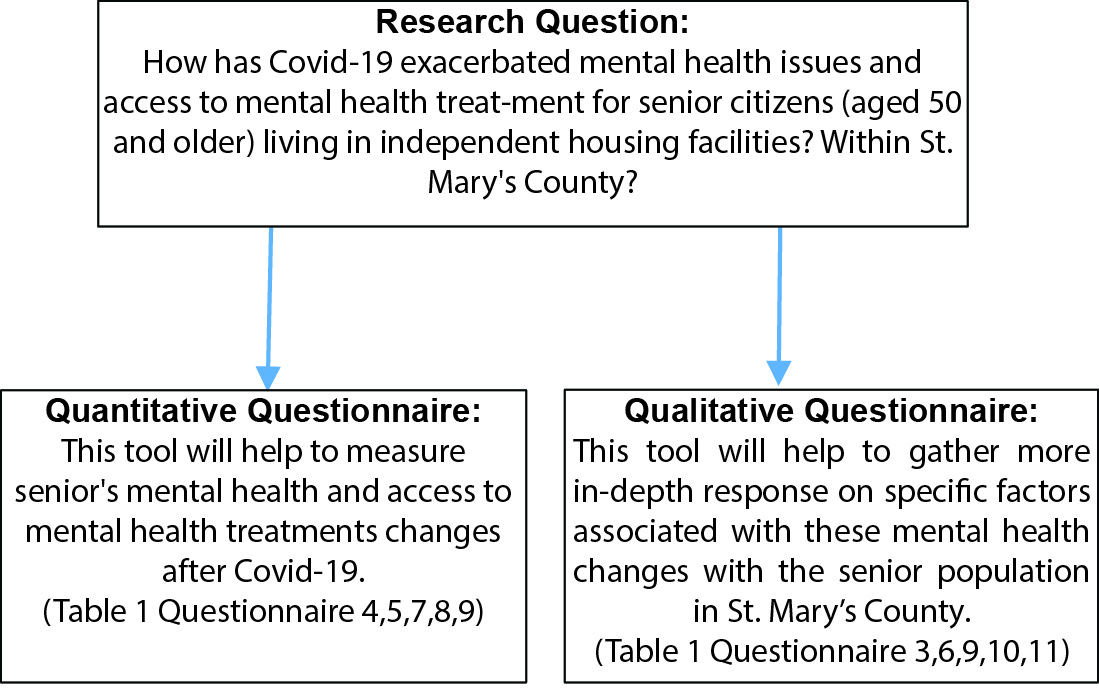
A two-part mixed-method study was conducted. This method allowed for both quantitative and qualitative data collection. The quantitative data provides the general scope of the research, and the qualitative data provides additional details on the opinions of senior citizens and their mental health. The two instruments used in the study were the quantitative survey questionnaire and the qualitative survey questionnaire. As previously mentioned, researchers have conducted research on the mental health and access to mental health treatment of senior citizens during Covid-19, but there is a lack of data surrounding this topic within rural communities like St. Mary’s County.
Participants.
The participants in this study were senior citizens (aged 50 and older) living in independent housing facilities within St. Mary’s County. The easiest way to access these populations in the county is through senior centers. This demographic was chosen because these seniors were deemed to have the greatest insights pertaining to the change in mental health due to the Covid-19 pandemic on senior citizens living in independent housing facilities. The survey questionnaire that was used in the study is shown in Table 1.
| Table 1. Participant Questionnaire | |
| Questions: | Responses: |
| 1. Do you consent to take the survey? | Yes/No |
| 2. I will ask the questions, and you just need to give a verbal response. Do you understand? | Yes/No |
| 3. Mental health includes our emotional, psychological, and social well-being. It affects how we think, feel, and act. What words come to mind when I say, “mental health”? | Negative/Positive & Explanation |
| 4. On an average day, rate your mental health before the pandemic from 1-10. (1 would be feeling hopeless, confused, depressed, emotionally drained, and socially secluded, and 10 feeling the best and happiest you ever have emotionally) | 1-10 |
| 5. On average, rate your mental health during the pandemic on a scale from 1-10. (1 would be feeling hopeless, confused, depressed, emotionally drained, and socially secluded, and 10 feeling the best and happiest you ever have emotionally) | 1-10 |
| 6. If your answer was different from the past two answers, what do you think caused these changes? (what during the pandemic caused this change in mental health) | Explanation |
| 7. Have you or another senior you know ever accessed mental health services/treatment? | Yes/No |
| 8. If yes, was it before the pandemic, during the lockdown, or after? | Before/During/After |
| 9. Was the mental health service easily accessible and helpful? Please explain if the answer is no and if there was difficulty accessing the service. | Yes/No & Explanation |
| 10. What do you think prevents senior citizens from getting the mental health services they need in St. Mary’s County, especially after the pandemic? | Explanation |
| 11. What kind of community support services would be helpful for senior citizens in their mental well-being and personal resilience, especially as we continue to deal with the Covid-19 pandemic? | Explanation |
Procedures.
The study design and procedures were approved by the Institutional Review Board. Once the project was approved, three senior center directors at Northern Senior Center, Loffler Senior Center, and Garvey Senior Center were emailed for possible dates for the administration of the survey. Directors that did not answer the email were given a call and left voice messages. Upon agreement, the directors provided dates and times for the administration of the survey to residents. Before the survey was given to the seniors, they were required to give verbal informed consent. To ensure confidentiality, the consent form informed participants that all surveys would remain anonymous. The survey was conducted in a separate area for each individual to have maximum privacy.
After obtaining all the data, the quantitative and qualitative questions were separately grouped. For quantitative data trends on mental health and access to mental health services, the survey responses will be grouped into categories. The ratings and opinions of the respondents were analyzed through numerical bar graphs to find correlated trends in the data. For qualitative data on mental health and access to mental health services trends, word choices were coded into positive/negative tones. Qualitative trends were further analyzed through language choices to examine emotional shifts over time through thematic analysis. This allowed for the analysis of the specific factors that caused mental health changes for senior citizens within St. Mary’s County.
RESULTS.
Quantitative results.
The survey questionnaire was completed by participants from three senior centers (Northern, Loffler, and Garvey) in St. Mary’s County. It’s important to note that only the responses of senior citizens that agreed to participate, were aged 50 and above, and lived in independent housing facilities were used in data analysis. The responses that did not meet these criteria were omitted.
The senior citizens’ mental health ratings were measured before the Covid-19 pandemic and during the Covid-19 pandemic. To be able to test if the difference in rating was statistically significant and did not occur by chance, a Chi-square test for homogeneity was used. The null hypothesis for this test states that there is no significant difference between the two mental health ratings before and during the Covid 19-pandemic. The alternative hypothesis states that there is a significant difference between the two ratings of mental health before and during the Covid 19-pandemic. Table 2 below shows all the mental health ratings grouped in the categories from 1-4, 5-7, and 8-10. There is a large number of ratings that dropped from the 8-10 category to the 5-7 category during the Covid-19 pandemic. Table 3 presents the expected values for each category, while Table 4 displays the test statistics, both derived using the Chi-square test for homogeneity. The Chi-square test for homogeneity compares observed data with expected data to see if different groups have the same distribution. The expected values are calculated based on the totals from each row and column, and the test statistic measures how much the observed and expected values differ. A higher test statistic value indicates greater differences between expected and observed values, leading to a higher possibility of rejecting the null hypothesis. The highest test statistics were found in the 5-7 and 8-10 categories directly correlating to the drop in mental health ratings. The Chi-square test showed a value approximately equal to zero, indicating that the null hypothesis should be rejected and that there is a significant difference between the two ratings of mental health before and during the Covid-19 pandemic.
| Table 2. Mental Health Ratings, from questions 4&5 in Table 1 | ||||||
| Observed | 1-4 | 5-7 | 8-10 | Total | ||
| Before Covid-19 | 0 | 7 | 56 | 63 | ||
| During Covid-19 | 10 | 32 | 21 | 63 | ||
| Total | 10 | 39 | 77 | 126 | ||
| Table 3. Expected Values, from questions 4&5 in Table 1 | ||||||
| Expected | 1-4 | 5-7 | 8-10 | |||
| Before Covid-19 | 5 | 19.5 | 38.5 | |||
| During Covid-19 | 5 | 19.5 | 38.5 | |||
| Table 4. Test Statistics, from questions 4&5 in Table 1 | ||||||
| Test Statistic | 1-4 | 5-7 | 8-10 | |||
| Before Covid-19 | 5 | 8.01282 | 7.9545 | |||
| During Covid-19 | 5 | 8.01282 | 7.9545 | |||
The senior citizens’ change in mental health services was also analyzed (Table 5). Out of the 63 responses from all three senior centers, only 30 of the seniors were using a mental health service or knew someone using it. 22 of those 30 seniors were already using the mental health service before the pandemic and 8 of them started using it during or after the pandemic. 3 of those 8 seniors stated that the mental health service was not easily accessible because of financial and availability issues. Less than 50% of the respondents were able to answer these questions, so the data is very limited in significance.
| Table 5. Senior citizens’ change in mental health services after the pandemic, based on responses to questions 7-9 in Table 1 | |
| 30/63 | Senior citizens knew others using a mental health service or were using one themselves |
| 22/63 | Senior citizens were already using a mental health service |
| 8/63 | Started using the mental health services during/after lockdown |
| 3/63 | Found the mental health service not helpful or not accessible |
Qualitative Results.
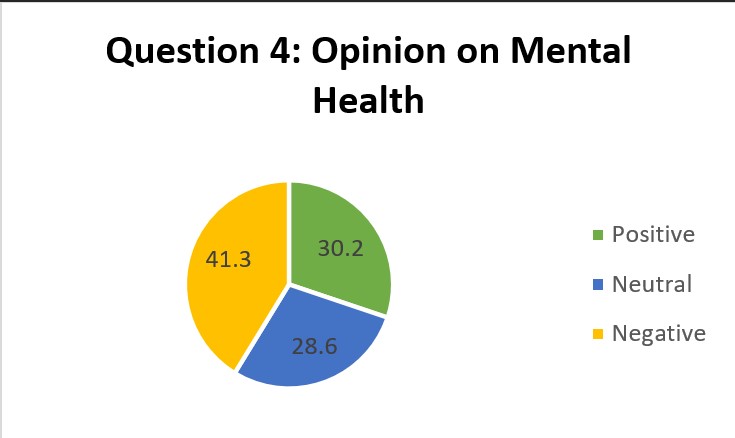
The qualitative results, questions 3,6,10,11 from Table 1ere coded in an open-coding format for each emerging theme. The senior citizen’s opinion on mental health was measured. Words that came into the senior citizen’s mind for mental health tended to be more harmful and neutral than positive toned (Table S1). 19/63 seniors gave mental health descriptions that were positive, 18/63 seniors gave mental health descriptions that were neutral, and 26/63 seniors gave mental health descriptions that were negative (Figure 2).
DISCUSSION.
This study was designed to examine how Covid-19 exacerbated mental health issues and access to mental health treatment for senior citizens (aged 50 and older) living in independent housing facilities within St. Mary’s County.
The results of this study revealed that there were multitude of factors that exacerbated the mental health of senior citizens in St. Mary’s County. Since St. Mary’s County is a rural area, there are factors that were more prevalent in this area than those conducted by researchers in more populated areas. Isolation leads to a lack of socialization, social networks affecting mental health, and emotional/physical issues caused by Covid 19 were the three main reasons for the drop in mental health for senior citizens (Table S2). The isolation can be connected to the closing of senior centers and other social activities for senior citizens during Covid-19. As these seniors were living by themselves in independent housing facilities, they were more likely to listen for information about Covid-19 on the news or other media networks. This uncertainty and fear of the unknown caused by Covid-19 and not having anyone to talk to could be further connected to emotional and psychological issues affecting senior citizens’ mental health.
There was also a multitude of factors that exacerbated access to mental health treatment for senior citizens in St. Mary’s County. This included neglect, lack of awareness, financial issues, lack of availability, emotional and physical issues, and lack of transportation (Table S3). In rural areas like St. Mary’s County, it is hard to communicate within the community, which could lead to a lack of awareness and neglected use of these mental health services. Many senior citizens believed that they did not need to access these services, even if it was necessary. Also, since there are fewer mental health treatment options in rural communities, Covid-19 only worsened access to these treatments specifically for senior citizens. Additionally, there are very few means of transportation for senior citizens in St. Mary’s County. The pandemic and temporary closing of transportation services made this a bigger issue as well.
CONCLUSION.
This study helps to address gaps in pre-existing research. Global attempts were made to address how the pandemic has affected the mental health and treatment of senior citizens. But there was a lack of research surrounding how Covid-19 affected the mental health of senior citizens in rural communities. Even more so, there was no research surrounding the negative impact of Covid-19 on seniors’ mental health in St. Mary’s County. The targeted subjects were senior citizens 50 and older living in independent housing facilities. This gap served as the main foundation for the research. Through surveys conducted at Northern, Loffler, and Garvey Senior Centers, the researchers gained insight to various reasons behind the exacerbation of mental health and access to mental health treatment for these senior centers. The main reasons found were isolation leads to a lack of socialization, social networks affecting the mental health of senior citizens, emotional/physical issues, neglect, lack of awareness, financial issues, lack of availability, and lack of transportation.
This study could help spur the local health department and other facilities that work with senior citizens to incorporate better mental health opportunities for senior citizens living in independent housing facilities. Those that were not previously aware of how Covid-19 worsened the mental health of seniors could now properly communicate and advocate for this population. By advocating for this population, fewer senior citizens would feel neglected or be misinformed about mental health and its significant importance. More facilities could incorporate activities and areas where the senior citizens could socialize and feel supported. This could also help limit the isolation that seniors feel, especially those that live in independent housing facilities (Table S4). St. Mary’s County could partner with other mental health organizations like the National Council on Aging and Substance Abuse and Mental Health Services Administration to provide more funding and accessibility of mental health services to senior citizens. Funding could help seniors access the mental health services they need at a low cost and have better access to various transportation options.
Only senior citizens from three senior centers were surveyed. There may be other senior citizens living in independent housing facilities within St. Mary’s County that do not attend these senior centers or facilities. The data collected also excludes people who are severely impaired because of the functional capabilities required to participate in the survey. Additionally, all seniors aged 50 and above were surveyed. Certain age groups may be underrepresented in the data collected from the three senior centers resulting in inaccurate results. If this research was repeated, other senior citizens could be studied to increase the sample size.
This study’s findings give way to new areas of research. The sample size can be expanded to include senior citizens living with family members, and not just those living in independent housing facilities. Additional research can also expand beyond St. Mary’s County to other rural communities in the United States and even North America or internationally. Rural counties tend to be more overlooked, so further research can be done within these small counties to find location-specific solutions (8). Other faculty and adults that are in frequent contact with senior citizens could also be an additional source of research and further analysis to find better solutions. Overall, obtaining more perspectives can help further insights into how Covid-19 affected and exacerbated mental health and access to mental health treatment for senior citizens.
ACKNOWLEDGMENTS.
I would like to express my heartfelt gratitude to my teachers and mentors for their invaluable guidance and support throughout this research project. I also extend my sincere thanks to the administrators and staff at the Northern, Loffler, and Garvey Senior Centers for allowing me to conduct my research in their facilities. Their cooperation and encouragement were instrumental in the success of my work. Lastly, I am grateful to my parents for their unwavering support and belief in me, which has inspired me to pursue my research with passion and dedication.
SUPPORTING INFORMATION.
The supporting information document includes:
- Data from question 3(Table S1): Mental health includes our emotional, psychological, and social well-being. It affects how we think, feel, and act. What words come to mind when I say, “mental health”?
- Data from question 6(Table S2): If your answer was different for the past two answers, what do you think caused these changes? (what during the pandemic caused this change in mental health)
- Data from question 10(Table S3): What do you think keeps seniors from getting the mental health services they need in St. Mary’s County, especially after the pandemic?
- Data from question 11(Table S4): What kind of community support services would be helpful for seniors in their mental well-being and personal resilience, especially as we continue to deal with the Covid-19 pandemic?
REFERENCES.
1.Impacts of Covid-19 on rural mental health. Morning Consult (2020). Available at: https://www.fb.org/files/Impacts_of_COVID-19_on_Rural_Mental_Health_1.6.21.pdf. Accessed August 15, 2024.
- Capriotti, T., Pearson, T., & Dufour, L. Health disparities in rural America: Current challenges and future solutions. Psychiatry Advisor (2022). Available at: https://www.psychiatryadvisor.com/features/health-disparities-in-rural-america-current-challenges-and-future-solutions/2/. Accessed August 15, 2024.
- Providing care for the underserved at MedStar St. Mary’s Hospital. American Hospital Association. Available at: https://www.aha.org/case-studies/2014-12-15-providing-care-underserved-medstar-st-marys-hospital. Accessed August 15, 2024.
- St. Mary’s County Community Health Assessment. Healthy St. Mary’s Partnership (2020). Available at: http://healthystmarys.com/wp-content/uploads/2020/12/2020-SMC-CHA-Report_1.pdf. Accessed August 15, 2024.
- Mitchell, C. Seniors and mental health. Pan American Health Organization / World Health Organization (2014). Available at: https://www.paho.org/en/topics/mental-health. Accessed August 15, 2024.
- About mental health. Centers for Disease Control and Prevention (2021). Available at: https://www.cdc.gov/mentalhealth/learn/. Accessed August 15, 2024.
- Heidinger T and Richter L. The Effect of COVID-19 on Loneliness in the Elderly. An Empirical Comparison of Pre-and Peri-Pandemic Loneliness in Community-Dwelling Elderly. Front. Psychol. 11, 585308 (2020).
- Gale, J., Janis, J., Coburn, A., & Rochford, H. (2020). Behavioral health in rural America: Challenges and opportunities. Rural Policy Research Institute. Available at: https://rupri.org/wp-content/uploads/Behavioral-Health-in-Rural-America-Challenges-and-Opportunities.pdf. Accessed August 15,2024.
Posted by buchanle on Wednesday, June 25, 2025 in May 2025.
Tags: COVID-19, Mental Health, Senior Citizens

