Exploring Clinician Confidence of Different Developmental Profiles While Using TAP-P
ABSTRACT
Due to long wait times, families are unable to access autism spectrum disorder (ASD) evaluations. For faster access to ASD evaluations, telehealth tools like the novel TELE-ASD-PEDS-Preschool (Telehealth Autism Spectrum Disorder Pediatrics- Preschool: TAP-P) were created. This prompted the need to research what profiles are fit for this tool. We hypothesized that clinician confidence rate will depend on the developmental profile of each child. We evaluated TAP-P to see what clinicians most rely on to diagnose ASD. Our experimentation consisted of analyzing clinician confidence in diagnosis, TAP-P scores given when giving diagnostic impression, and clinician perception. To view clinician perception, we split the scoring tool of the TAP-P into two sections: Restrictive Repetitive Behaviors (RRBs), and Social Affect (SAs). RRBs are behavior indicators that are commonly seen in in-person evaluations for ASD. We found that clinicians will only give a diagnostic impression of ASD if they are confident in their answer. Clinicians giving a higher TAP-P score also appeared to be correlated to a diagnostic impression of ASD. In relation to clinician confidence, we found that clinicians perceived that they heavily relied on RRBs when making a diagnostic impression. When we looked at what clinicians mostly used based on their recorded impressions, we found that 75% of the RRBs were used.
INTRODUCTION.
For a long time, ASD has mostly been diagnosed in person. The in-person diagnosis, Autism Diagnosis Observation Schedule- 2 (ADOS-2) has been what families rely on to get results. This has made the entire process for diagnosing ASD very difficult. It has made the wait times years long. For the ADOS-2 [4], if you reach a certain age, sometimes there will be an age cut off within clinics, and then a toddler will be unable to receive a diagnosis. Due to there being an age cut off, more toddlers would be waiting for a long time and then lose their spot because they got older, therefore making someone else wait far longer. This was frustrating to the families because they were not getting a diagnosis, any resources, and wasting time on a waitlist that was uncertain. Another issue we wanted to address is getting more access to families who do not live near a clinic. At times, there will only be one or maybe two clinics near the patient making it too far of a drive, or families cannot call out of work to show up in person.
Due to these wait times, and wait times around overall health, telehealth has been something that clinicians are learning to use. Telehealth can be a variety of things: a doctor’s appointment, a therapy appointment, or an ASD evaluation. With telehealth and the TELE-ASD-PEDS (Telehealth Autism Spectrum Disorder Pediatrics: TAP) [1] in mind, the TAP-P was created. This was meant to help families get a quicker diagnosis for their child before the age cut off. [2] We hope that telehealth will allow for more people to get the help they need sooner.
The TELE-ASD-PEDS-Preschool (TAP-P) is a clinician-guided, parent-led telehealth tool used to screen for ASD in children aged 36 to 72 months.
It was adapted from the original TELE-ASD-PEDS (TAP). The TAP-P is a play-based activity that allows for clinicians to look at behavior and social interactions of a toddler. To better understand what profiles are fit for TAP-P, we examined clinician confidence with various aspects of the tool. We hypothesized that clinician confidence rate will depend on the developmental profile of each child.
MATERIALS AND METHODS.
Procedures.
Participants were recommended by pediatricians and other third parties. Families were contacted through a phone call and informed of the contents of research, compensation, forms of communication and paperwork needed. The communication would be sent through an email, summarizing the call and any other additional information.
Telehealth Visit.
First, a telehealth visit consisting of the TAP-P administration is held. This telehealth visit is a recorded Zoom meeting (only TAP-P administration was recorded) and could be joined from a phone, a tablet, or a computer. Families were asked to only have the toddler that would be evaluated in the room along with the caregiver(s). The meeting would generally include one clinician, the person that guided families through the process and sent out all the information, and the family.
Tele-assessment.
The TAP-P consists of several play-based activities as well as some interactive activities. These activities were discussed in the email that was originally sent out to families. They were asked to prepare a specific list of toys and supplies that could be used during the administration. The toys would be used to have free play and structured play. Some snacks would be used for interactive activities. Free play consisted of several parts. One, seeing how the toddler plays by themselves; allowing us to see if they socialize with others or portray any clear signs or behaviors that might code for ASD. Free play also consists of playing with a caregiver without instruction. This helps clinicians see how well their social skills are as well as their quality of interaction. Structured play would consist of playing with a caregiver with instructions from clinicians. Things like rolling toys back and forth or building something would be considered structured play. Then, came some interactive activities: toddler asking for help opening a snack, clinicians taking turns with toddler drawing, or asking what emotion the toddler saw when clinician shared their screen with pictures of other toddlers. After the TAP-P is over, a Diagnostic Profile-4 (DP-4) [3] is preformed: a parent interview that asks caregivers about their concerns, what clinicians might not have seen, motor skills, and social skills.
Post Visit.
After this visit, another email is sent to families for when their second in-person visit will be for their official evaluation with the validated tool, ADOS-2. An email was sent to clinicians asking them to rank the item tasks on a rating form, from most to least important, measured in terms of their confidence when giving diagnostic impressions. Each of the item tasks were divided into two categories: Restrictive Repetitive Behaviors (RRBs), or Social Affects (SAs). They were divided into these sections because RRBs were much more perceptible signs while SAs were harder to perceive. The RRBs consisted of speech abnormalities, repetitive interests or behaviors, characteristic or repetitive body movements, and sensory exploration or reaction. Clinicians used these signs to reaffirm their diagnostic impression. When speaking with clinicians, they expressed that they felt more confident using the RRBs to reaffirm their impressions due to the complexity of the SAs. With the responses clinicians provided, we made charts that allowed us to see how similarly clinicians thought.
RESULTS.
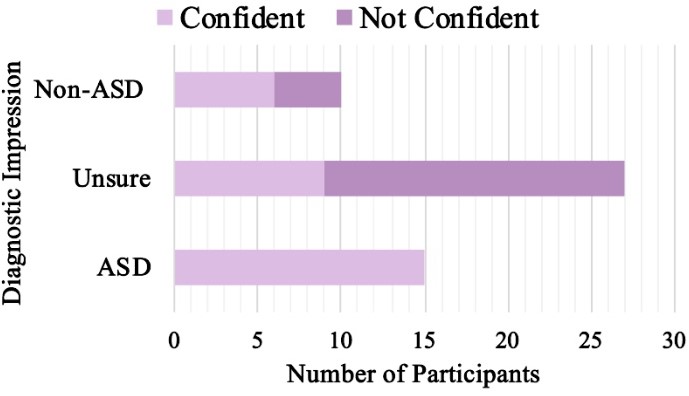
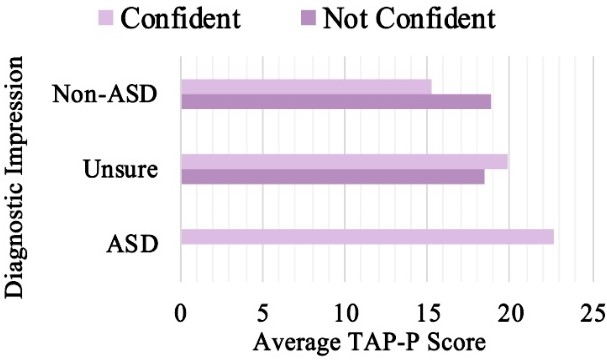
We found in Figure 1 that there are more participants that will get a diagnostic impression from a clinician that is completely certain in comparison to an uncertain clinician’s diagnostic impression. Figure 2 shows the higher the TAP-P score, the more likely it will be that the diagnostic impression will result in ASD.
We found in Table 1 that clinicians score higher ratings on RRB item tasks when ASD is present and when confidence rate is high. Table 2 shows clinicians score higher ratings on RRB item tasks (bolded) when ASD is present and when confidence rate is high. Clinicians perceive RRB item tasks to be important to their diagnostic impression. When we looked at what clinicians mostly used based on their recorded impressions, we found that 75% of the RRBs were used in comparison to the 50% within the highest scored tasks.
| Table 1. Clinician Confidence in Correlation to Diagnostic Impression | ||||
| Rating Items (Likert scores) | ASD present (n=14) | ASD unsure (n=27) | Non-ASD (n=10) | Confident Clinicians (n= 29) |
| RRB (1,2,3) | 2.00 | 1.54 | 1.30 | 1.74 |
| SA (1,2,3) | 1.83 | 1.60 | 1.39 | 1.65 |
| Confidence Ratings | ||||
| Average Confidence Rate (1,2,3,4) | 3.21 | 2.11 | 2.80 | 3.17 |
| Table 2. Clinician Ranking of Tasks in Order of Importance to Diagnostic Confidence vs. Highest Scored Tasks of Most Confident Diagnostic Impressions | |||
| Top 4 Ranked Tasks | Perception of Importance to Diagnostic Confidence | TAP-P Scores (1,2,3) | Highest Scored Tasks of Most Confidence Diagnostic Impressions |
| 1 | Quality of social interactions | 2.17 | Speech abnormalities |
| 2 | Speech abnormalities | 2.10 | Conversation |
| 3 | Repetitive interests or behaviors | 1.96 | Interactive pretend play |
| 4 | Characteristic or repetitive body movements | 1.93 | Repetitive interests or behaviors |
DISCUSSION.
In trying to find what would help clinicians gain a better understanding of what might help their confidence in their diagnostic impressions, we found that they rely on a child’s developmental profile. The first thing we take note of, is that there were no clinicians that would give a diagnostic impression of ASD if they were unsure. This is important because it allows us to understand why we can further trust these tools. In relevance to that, we saw that the average TAP-P scores allow clinicians to feel confidence in their diagnostic impressions, demonstrating that there is a correlation between scores, confidence and diagnostic impressions for the TAP-P. We also found that RRBs and SAs can be a great help to clinician confidence. It allows for clarification and certainty when making a diagnostic impression. One thing we would like to keep in mind for future research is expanding the number of clinicians that were part of the study. Knowing that clinicians can have a different perspective to help make their diagnostic impression, we found that they perceive themselves to use more RRBs, however statistically, they use a mix of both RRBs and SAs. On a larger scale, we see that there is a potential profile that can be used to determine who is fit to have a diagnostic impression with the TAP-P.
CONCLUSION.
Clinicians do rely on the developmental profile of each child to make a diagnostic impression. In relation to clinician confidence, we found that clinicians perceived that they heavily relied on RRBs when making a diagnostic impression. Clinicians reported parent interviews to be highly important in their diagnostic impressions. In the future, we would like to find a way to make this tool available to children who have more social skills and do not show clear signs of ASD, such as, further developed, developmental profile. Future research should continue to target older children with varied developmental profiles.
ACKNOWLEDGMENTS.
Research was supported by the National Institute of Health under Grant Number R21MH128790, the Vanderbilt Treatment and Research Institute for Autism Spectrum Disorders, and the School for Science and Math at Vanderbilt. A special thank you to Dr. Zachary Warren, Alison Vehorn and Ambar Muñoz Lavanderos.
REFERENCES.
- Wagner, L., Corona, L. L., Weitlauf, A. S., Marsh, K. L., Berman, A. F., Broderick, N. A., Francis, S., Hine, J., Nicholson, A., Stone, C., & Warren, Z., Use of the TELE-ASD-PEDS for Autism Evaluations in Response to COVID-19: Preliminary Outcomes and Clinician Acceptability. Journal of Autism and Developmental Disorders 51, 3063–3072 (2020)
- Wagner, L., Vehorn, A., Weitlauf, A. S., Lavanderos, A. M., Wade, J., Corona, L., & Warren, Z., Development of a Novel Telemedicine Tool to Reduce Disparities Related to the Identification of Preschool Children with Autism. Journal of Autism and Developmental Disorders 55, 30–42 (2023).
- Ozonoff, S., Gangi, D., Corona, L., Foster, T., Hill, M. M., Honaker, M., Maqbool, S., Ni, R., Nicholson, A., Parikh, C., Stone, C., Spitler, A. K., Swanson, A., Vehorn, A., Wagner, L., Weitlauf, A., & Warren, Z., Measuring Developmental Delays: Comparison of Parent Report and Direct Testing. Journal of Autism and Developmental Disorders, 27, 1-7(2024).
- Colombi, C., Fish, A., & Ghaziuddin, M., Utility of the ADOS-2 in children with psychiatric disorders. European Child & Adolescent Psychiatry, 29, 989–992 (2020).
Posted by buchanle on Thursday, June 19, 2025 in May 2025.
Tags: Autism Spectrum Disorder (ASD), Developmental Profile, Restrictive Repetitive Behaviors (RRBs), TELE-ASD-PEDS-Preschool (Telehealth Autism Spectrum Disorder Pediatrics- Preschool: TAP-P), Tele-assessment

