Faculty Use Universal Language of Math to Tackle Some of COVID-19’s Biggest Challenges
As public health officials tackle the COVID-19 pandemic, they face an overwhelming number of factors that affect the virus’s spread. Population density, economic challenges, adherence to social distancing measures—they all play a part in determining the rise or fall of infection rates. And the results of efforts to “flatten the curve” can vary from place to place. So, how to make sense of it all? How do we manage the virus? The answer might lie in the universal language of math.
 Two faculty members in the Department of Mathematics have spent the past few months addressing some of the most pressing issues in the fight against COVID-19. Professor of Mathematics Glenn Webb has been making a predictive mathematical model to project the spread of the virus in different locations. Research Professor of Mathematics Philip Crooke has seen a resurgence in the use of an online ventilator simulator he helped develop a few years ago. Together, these faculty are making a real-time impact on how we understand and treat COVID-19.
Two faculty members in the Department of Mathematics have spent the past few months addressing some of the most pressing issues in the fight against COVID-19. Professor of Mathematics Glenn Webb has been making a predictive mathematical model to project the spread of the virus in different locations. Research Professor of Mathematics Philip Crooke has seen a resurgence in the use of an online ventilator simulator he helped develop a few years ago. Together, these faculty are making a real-time impact on how we understand and treat COVID-19.
Webb’s project approaches COVID-19 from a global perspective. In the early weeks of the pandemic, he and his colleagues examined data from around the world about how the virus was spreading, rates of infection and the safety measures different governments were implementing. The researchers then started building a predictive model for the virus to see if they could accurately project future cases. This required a tremendous amount of intricate and complicated work, but Webb and his team were determined to create a model that could be validated against case data—and he thinks they’ve done it.
“We’ve managed to build a very simple model that has the elements of the epidemic and is a good fit for the data. That’s what we want—a model that we can project forward, and then can be updated as time advances. You can update your position and see if things are going right or not and modify accordingly,” Webb said.
Their model uses differential equations to analyze reported case data and predict the future number of cases in specific locations by incorporating three important elements of COVID-19: (1) the number of asymptomatic infectious individuals (with very mild or no symptoms), (2) the number of symptomatic reported infectious individuals (with severe symptoms), and (3) the number of symptomatic unreported infectious individuals (with less severe symptoms).
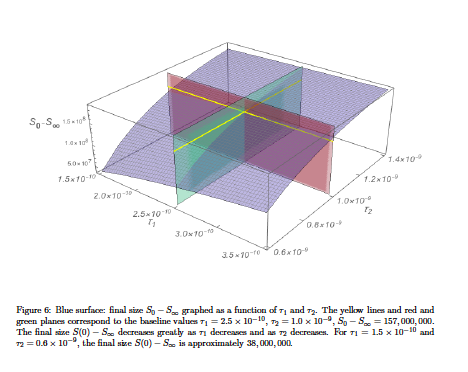
The model also segments the pandemic into three phases, based on the virus’s rates of increase or decrease. These phases are meant to indicate both the level of infection in an area and the level of success in controlling the spread of the virus. Various parameters add further specificity to the model. For instance, the model can account for the intensity and effectiveness of preventive measures, such as physical distancing, and predict how they might help decrease infection rates. With countries in various states of reopening, this kind of prediction is especially useful right now. That’s the value of the models, Webb said. Because of a lack of widespread testing earlier in the pandemic, Webb has not yet applied the model to the United States. However, recent increases in domestic testing give him hope that the model will prove useful here at home. From major metropolitan areas to states, regions and the country as a whole, Webb hopes to get a glimpse of what the future might hold as officials loosen safety measures and try to return to normal.
Webb and his team have submitted their model to academic journals, but the publication process can take a year or more. To ensure that policy teams have access to the model now, while they are actively making reopening decisions, the team has posted archival versions online.
“What good is a model that appears a year from now?” Webb said. “If it’s ready today, we want it up and going tomorrow.”
Phillip Crooke, meanwhile, has used his expertise in biomathematics to train frontline health care workers in a vital skill: how to use a mechanical ventilator. A differential equation model powers the mechanical ventilator simulator, which selects a random chart from more than 100 virtual patients, and the trainee must then make adjustments to the ventilator to stabilize the patient.
Crooke created the simulator a few years ago with his colleague John Hotchkiss, an associate professor of critical care medicine and medicine at the University of Pittsburgh—a connection he made nearly 25 years ago through a colleague in Vanderbilt’s School of Medicine. But at the time of its creation more than three years ago, there wasn’t much immediate need for a ventilator simulator model. Crooke and Hotchkiss put it online anyway, where it received four or five downloads per week. But in March 2020, when COVID-19 began to spread across the U.S., that number started to climb to 100-200 downloads per day.
Because the simulator is written in Visual Basic using a Microsoft Excel spreadsheet, it has the added benefit of being both self-contained and a practical training tool—it can run on an average computer.
“It’s accessible by anybody. If you look at where our downloads are coming from, it’s all across the world: the U.S., South America, Europe, Africa,” Crooke said. “Especially in countries where there’s not a lot of training available, this is a cheap and direct way for them to get trained, especially if they are using it in conjunction with an online ventilator course.”
Crooke is thankful that this model has found its way into the hands of more health care workers and that it is available to them, for free, exactly when they needed it. He credits models like this to the collaborative environment at Vanderbilt. Working on biomathematical models requires mathematicians and physicians or biological scientists to work in tandem, using their expertise to solve the problem together. Crooke said these types of biomathematics partnerships almost always seem to happen because faculty members are bold enough to walk across campus, knock on each other’s doors and ask questions.
“Almost every collaboration I’ve had has started that way,” Crooke said. “And it’s one of the greatest features of our university.”
