Researchers discover method to make traditional topical antibiotic safe to inject, potentially reducing antibiotic resistance
After scraping your knee or getting cut by an errant tree branch, you likely slathered your injury with the antibiotic ointment Neosporin.
Widely used to prevent infection, one of the active ingredients in Neosporin is neomycin. Discovered in the 1940s, neomycin is an effective topical antibiotic, however, if injected into the body to treat systemic infections, it can cause deafness, kidney damage, and neurological damage.

In a new study published in Nature Cell Biology, Research Assistant Professor of Biological Sciences Bhawik Jain and his colleagues determined why some human cell types are adversely affected by neomycin and how removing the lipid phosphatidylinositol-4-phosphate (PI4P), which transmits information within and between cells, can make neomycin a safe and effective drug injection. This discovery could help fight antibiotic-resistant bacteria—a global public health threat according to the Centers for Disease Control and Prevention.
The team studied a family of proteins called P4-ATPases, which transport specific lipids from the outer to the inner membrane of cells. These proteins are essential for healthy cell function in the human body. Defects in P4-ATPases are linked to various human diseases, including severe neurological disorders.
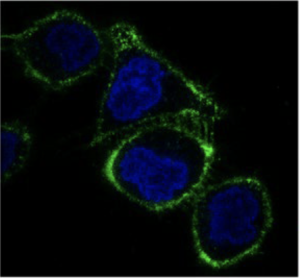
During their experiments, Jain and his team used yeast as a model organism, which contains the protein Neo1 that is similar to the human proteins ATP9A and APT9B. When Neo1 presented a defect, it would cause the lipid PI4P to appear in the outside layer of the cell membrane even though it is normally housed within. This allowed neomycin to bind to the lipid and enter the cell, causing adverse effects.
In humans, cells that normally express low levels of ATP9A and ATP9B, like kidney cells, expose PI4P on the outside of the membrane, which makes these cells sensitive to neomycin.

“It is essential to understand the mechanisms of antibiotic resistance in order to develop more effective drugs,” said Todd Graham, Stevenson Chair of Biological Sciences and senior communicating officer of the study. “We knew that Neo1 played an important role in antibiotic resistance, and we finally—after several years of research and multiple publications on this topic—developed a sufficient set of tools to crack the problem. It should be possible to remove PI4P from the outer layer of the plasma membrane of human cells and make them resistant to the drug while the bacteria remains sensitive.”
Moving forward, the team plans to test various ways to remove PI4P from the outer layer of kidney cells to protect them from neomycin, as well as to test the importance of PI4P for human cell sensitivity to other antibiotics. In doing so, they will be able to find additional treatments to fight antibiotic-resistant bacteria.
Read the full study on Nature Cell Biology’s website.
The study was published open access through a transformative agreement negotiated by Vanderbilt University’s Jean and Alexander Heard Libraries. Transformative agreements eliminate traditional paywalls and remove the obstacle of article processing charges, ensuring immediate and unrestricted access to research worldwide. Vanderbilt authors can learn more about the Heard Libraries’ agreements supporting open access publishing in this research guide.
